You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Alternate Day Fasting
- Thread starter Bribie G
- Start date

Help Support Australia & New Zealand Homebrewing Forum:
This site may earn a commission from merchant affiliate
links, including eBay, Amazon, and others.
Snow said:Whatever you do, don't go on anti-cholesterol drugs! The side effects of statins aren't worth it. Do your research before your doctor dictates what happens to your body. You need cholesterol, as the reason our bodies produce it and retain dietary cholesterol is to treat inflammation. There is lots of evidence that this inflammation is caused by carbs, sugar and omega 3/6 imbalance.
Have a look at these articles, for starters:
http://www.greenmedinfo.com/blog/there-only-one-type-cholesterol-heres-why
[SIZE=8pt]http://articles.mercola.com/sites/articles/archive/2010/08/10/making-sense-of-your-cholesterol-numbers.aspx[/SIZE]
[SIZE=8pt]http://articles.mercola.com/sites/articles/archive/2010/07/20/the-truth-about-statin-drugs-revealed.aspx[/SIZE]
I have changed my eating habits in tune with Nora Gedgaudas' approach (see www.primalbody-primalmind.com and get the book), but I am not religious about it - I have lapses, but try to minimise them. Basically I have cut out most carbs (no potato, rice, bread, cereal, pasta etc) and minimise sugar and fruit intake. I eat moderate amounts of red and white meat, fat, lots of vegies, fish and krill oil. I try for 3 AFDs a week, and have changed the WAY I excercise - eg, I used to go for a 25 min jog 2-3 times a week, but now I do 10-15 mins high intensity interval training (30 secs on, 90secs off x 6-8). Since I started this approach in January this year, I have dropped from 98kg to 85kg (thats right - 13kgs in 18 weeks). I feel great, don't get cravings, sleep better, sweat less, feel more alert and have had to get a new wardrobe. I'm still losing about a kilo a fortnight, so I don't know where it will end..... and i still drink plenty of beer, wine and whiskey! :chug:
Cheers - Snow.
You might want to try reading some articles from credible sources rather than the ones written by Natropaths, life coaches? and Dr Mercola.
Snow
Beer me up, Scotty!
- Joined
- 20/12/02
- Messages
- 2,349
- Reaction score
- 154
You might want to try and be civil and acknowledge that there are plenty of sources of information out there and "credibility' is entirely subjective unless, of course, they have been backed up by independent peer-reviewed scientific studies. I have read plenty of sources from doctors, WHO, Healthy Heart Foundation, university studies, etc, in addition to the links I provided in my post. The reason I provided those links is that they give an easy to understand explanation of what cholesterol does and doesn't do, and doesn't dumb down the message to "cholesterol bad, low fat good". The studies that Dr Mercola et al uses to base his opinions on are entirely "credible" and have been backed by peer-reviewed duplicate studies. Besides, why do you assume a naturopath can't summarise scientific facts in easy-to-read accessible articles?pcmfisher said:You might want to try reading some articles from credible sources rather than the ones written by Natropaths, life coaches? and Dr Mercola.
Snow said:You might want to try and be civil and acknowledge that there are plenty of sources of information out there and "credibility' is entirely subjective unless, of course, they have been backed up by independent peer-reviewed scientific studies. I have read plenty of sources from doctors, WHO, Healthy Heart Foundation, university studies, etc, in addition to the links I provided in my post. The reason I provided those links is that they give an easy to understand explanation of what cholesterol does and doesn't do, and doesn't dumb down the message to "cholesterol bad, low fat good". The studies that Dr Mercola et al uses to base his opinions on are entirely "credible" and have been backed by peer-reviewed duplicate studies. Besides, why do you assume a naturopath can't summarise scientific facts in easy-to-read accessible articles?
The woman that wrote the linked Greenmedinfo article is Heidi Stevenson. A quick google of her credentials shows she produces http://www.gaia-health.com/. Have a look at the site and tell me if she is someone worth listening to on anything remotely medical.
I will not be civil when it comes to bat **** crazy anti vaxing whack jobs.
Also, I am not interested in Dr Mercola's "opinions"? His summing up of
For the majority of you reading this right now, there's no reason to risk your health with cholesterol-lowering drugs. With the plan I've just outlined, you'll achieve the cholesterol levels you were meant to have, along with the very welcome "side effects" of increased energy, mood and mental clarity.
Too good to be true?
Hardly.
For the vast majority of people, making a few lifestyle changes causes healthy cholesterol levels to naturally occur.
is just plain rubbish.
Another quick search gives me http://www.docsopinion.com/2012/06/19/should-i-take-cholesterol-lowering-drug-2/
and a couple of publications you will find therein.
http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2812%2960367-5/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/14692706
These are what you call credible scientific sources. Nowhere can I read -
Whatever you do, don't go on anti-cholesterol drugs! The side effects of statins aren't worth it.
Why would you rely on a naturopath for scientific facts?
WarmBeer
Unhappy camper
felten said:Many of our ancestors were probably cannibals as well, how come no one is trying that diet?
bum
Not entitled to an opinion
- Joined
- 19/2/09
- Messages
- 11,585
- Reaction score
- 911
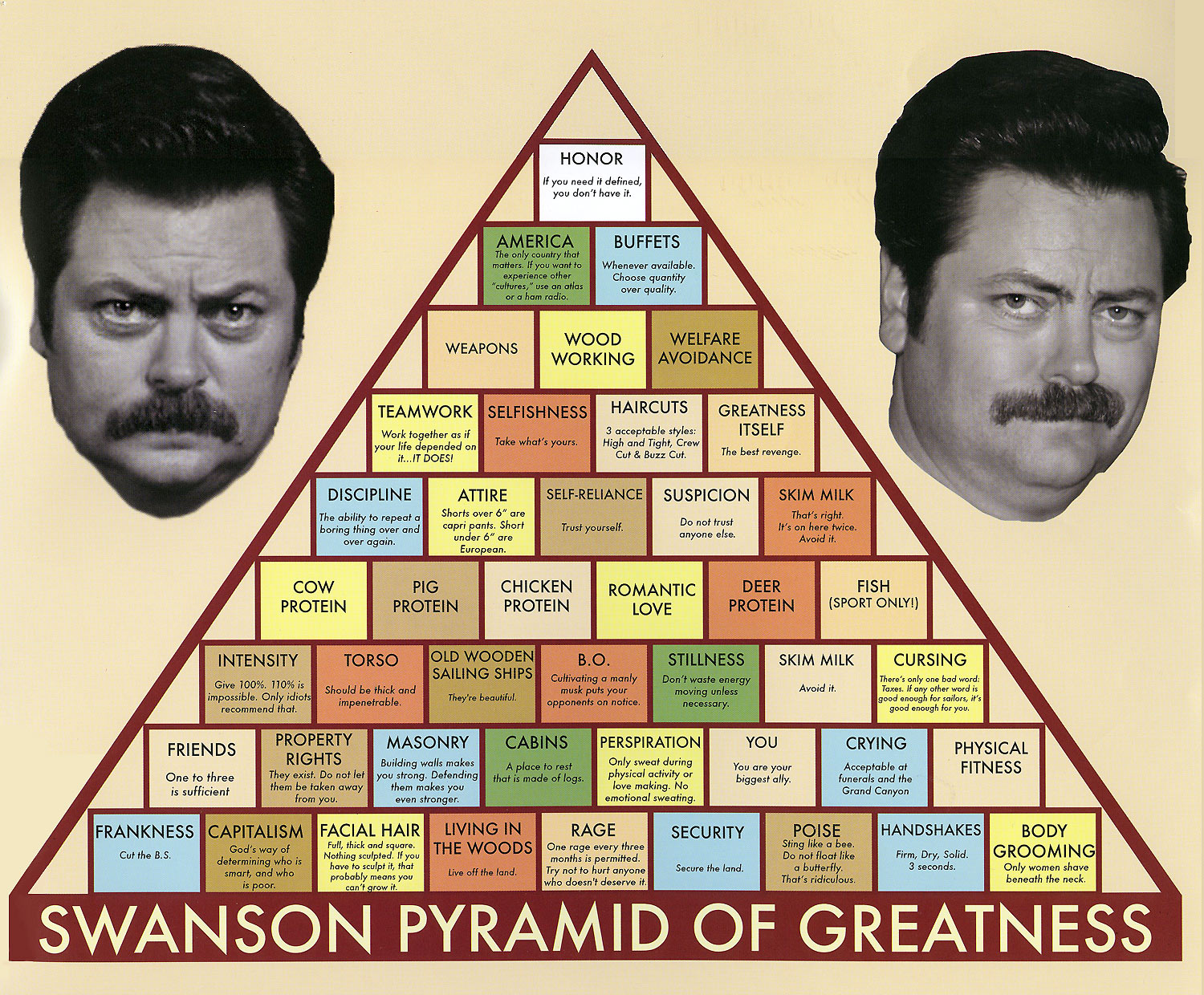
This has got to be the fifth time I've seen you mention this.Bribie G said:I wouldn't rely on the Government for the food pyramid (generated by scientists, sorry did I mention Monsanto?) that's presided over the fattest generations in human history.
AF_Food_Pyramid_52939.jpg
But then of course they are there to help us, not so?
Has anyone EVER constructed a meal around it? It is completely irrelevant to everyone's life. It most certainly did not produce the fattest generation ever.
manticle
Standing up for the Aussie Bottler
Eat less (smaller portions). Eat less fat. Eat less processed food. Eat less snacks. Eat more fresh food. Eat more regular meals. Exercise more often. Intensify your exercise. Exercise regularly.
Odd idea I know but seems to work.
Or cut out fruit and eat loads of red meat. I know which one makes sense to me.
Odd idea I know but seems to work.
Or cut out fruit and eat loads of red meat. I know which one makes sense to me.
GuyQLD
Well-Known Member
- Joined
- 13/5/12
- Messages
- 504
- Reaction score
- 152
I read the entirety of http://www.docsopinion.com/2012/06/19/should-i-take-cholesterol-lowering-drug-2/ And..... the comments... As bad as Youtube.
Works for youmanticle said:Eat less (smaller portions). Eat less fat. Eat less processed food. Eat less snacks. Eat more fresh food. Eat more regular meals. Exercise more often. Intensify your exercise. Exercise regularly.
Odd idea I know but seems to work.
Or cut out fruit and eat loads of red meat. I know which one makes sense to me.
So don't tell the relatively few on the forum, tell it to the billion people on the planet who aren't as disciplined and wise as you are. As for eating less fat, I think you have totally missed the point. Anyway I'm not going to post on this thread again, I'll start a blog with updates.
manticle
Standing up for the Aussie Bottler
How is eating better any less difficult than not eating for an entire day? followed by having 3 portions of chips + 1 egg and a wafer every tuesday but only one mandarin every alternate month?
Works for loads of people Bribie and has very simple science behind it.
Eat less fat is obviously very simplistic and there are good and 'bad' fats but beyond that, the above is pretty straight forward. Of course it requires effort but what doesn't? I'm surprised to see you falling for faddish type stuff bribie but I hope it works for you regardless.
Next you'll be telling me you want to change your name to Alistair.
Works for loads of people Bribie and has very simple science behind it.
Eat less fat is obviously very simplistic and there are good and 'bad' fats but beyond that, the above is pretty straight forward. Of course it requires effort but what doesn't? I'm surprised to see you falling for faddish type stuff bribie but I hope it works for you regardless.
Next you'll be telling me you want to change your name to Alistair.
matho
The Braumiser
- Joined
- 30/4/08
- Messages
- 1,403
- Reaction score
- 142
Manticle, I have done exactly that, eat less Kj and exercise more. I have been doing that since the end of feburay and have gone from 98kg to 80 kg and my resting heart rate has gone from 80 bpm down to 60 bpm. I ride my bike for at least 25 min a night (living in the mountains it gives you quite a work out) and I stay away from fried foods. I still have a little further to go in the weight loss but not far now.
joshuahardie
Beer, so much more than a breakfast drink
- Joined
- 8/5/07
- Messages
- 1,039
- Reaction score
- 38
But sadly it is the truth. Gotta eat less.Bribie G said:The "eat less" advisors are a bit like me saying "give up smoking, it's dead easy".
I have half heartedly tried to lose weight for years. Tried a few gimmicks, tried to over compensate for the food I ate with more exercise, and even tried not drinking.
Nothing really had an affect.
It was not the quality of the food that I was eating, I was eating quite healthy, but the proportions were too large.
Like Mike C, I was put onto MyFitnessPal, which does nore care to much for fat and sugar values, but is based on overall calorie intake. Despite my sckeptisicm, calorie counting really made me accountable for the quality and quantity of the food I put in my mouth, and like Matho I am averaging about 25 mins of exercise 4-5 times a week. It is not like I am missing out on food, but swapping out high calorie versions of food for low calorie versions of the same thing.mikec said:I used an iphone app called Myfitnesspal, which helps you keep track of your calories and exercise and your goals. Don't have an iphone? Just use the website.
I am down 7 kilos this year, and I hope I can push through and get rid of a couple more. I have not had a checkup to see if the ol' insides are any better, but I have taken almost 3 inches off my waist.
Go ahead and let us know how the fasting diet works, but it just seems like another fad to me.
manticle
Standing up for the Aussie Bottler
Got a mate who is a fellow brewer who was a reasonably hefty size when I met him. More recently we started playing futsal together - play weekly and train weekly. As a result of that his diet changed drastically and his exercise regime now includes riding a push bike and more importantly - weight training.Manticle, I have done exactly that, eat less Kj and exercise more. I have been doing that since the end of feburay and have gone from 98kg to 80 kg and my resting heart rate has gone from 80 bpm down to 60 bpm. I ride my bike for at least 25 min a night (living in the mountains it gives you quite a work out) and I stay away from fried foods. I still have a little further to go in the weight loss but not far now.
He's dropped over 30 kg in around 8 months and as a result is happier, fitter, more co-ordinated and looks much healthier.
One anecdote doesn't make a truth but there's more than anecdotal evidence to suggest that the right combination of eating the right things, regularly in appropriate portions and exercising regularly with some intensity leads to long term weight loss and health benefits.
No skin off my nose if people want to base their diet around that of a homo-erectus or a 12th century eskimo or eat pancakes on the eighth of every month, alternating between jam and marmalade every third round and if it works for you then go for it. It just seems like a massive overcomplication of a fairly simple equation. Yes there are things that make it more complicated like genetics, metabolic rates, etc but starving for a week, then eating cos lettuce on fridays and praline icecream on Sundays doesn't really seem like it's going to circumvent any of this.
Airgead
Ohhh... I can write anything I like here
- Joined
- 6/4/05
- Messages
- 3,651
- Reaction score
- 1,055
There is a teeny, tiny bit of very early speculative science that might show that intermittent fasting might just maybe have a positive effect on insulinlike growth factors. Maybe. And the same research shows that high protein diets are bad for IGF levels. And it specifically says that its not about losing weight but about cancer prevention (not that that's a bad thing), diabetes and other stuff.
There was a good article on it in New Scientist a few months back. I'll post the text below. If you have access to their site it has links to some of the primary sources.
I might wait a little while until someone actually shows that it works. In the mean time -
Eat Food
Not too Much
Mostly vegetables
or even simpler
Eat less
Move more.
*************************************************************************************************************************
For a healthier body and mind, forget food fads and try the age-old practice of going without
THERE'S a fuzz in my brain and an ache in my gut. My legs are leaden and my eyesight is blurry. But I have only myself to blame. Besides, I have been assured that these symptoms will pass. Between 10 days and three weeks from now, my body will adjust to the new regime, which entails fasting for two days each week. In the meantime, I just need to keep my eyes on the prize. Forget breakfast and second breakfast, ignore the call of multiple afternoon snacks, because the pay offs of doing without could be enormous.
Fasting is most commonly associated with religious observation. It is the fourth of the Five Pillars of Islam. Buddhists consider it a means to practise self-control and advocate abstaining from food after the noon meal. For some Christians, temporary fasts are seen as a way of getting closer to God. But the benefits I am hoping for are more corporeal.
The idea that fasting might be good for your health has a long, if questionable, history. Back in 1908, "Dr" Linda Hazzard, an American with some training as a nurse, published a book called Fasting for the Cure of Disease, which claimed that minimal food was the route to recovery from a variety of illnesses including cancer. Hazzard was jailed after one of her patients died of starvation. But what if she was, at least partly, right?
A new surge of interest in fasting suggests that it might indeed help people with cancer. It could also reduce the risk of developing cancer, guard against diabetes and heart disease, help control asthma and even stave off Parkinson's disease and dementia. Many of the scientists who study fasting practise what they research, and they tell me that at my age (39) it could be vital that I start now. "We know from animal models," says Mark Mattson at the US National Institute on Aging, "that if we start an intermittent fasting diet at what would be the equivalent of middle age in people, we can delay the onset of Alzheimer's and Parkinson's." Surely it's worth a try?
Until recently, most studies linking diet with health and longevity focused on calorie restriction. They have had some impressive results, with the lifespan of various lab animals lengthened by up to 50 per cent after their daily calorie intake was cut in half. But these effects do not seem to extend to primates. A 23-year-long study of macaques found that although calorie restriction delayed the onset of age-related diseases, it had no impact on lifespan. So other factors such as genetics may be more important for human longevity too (Nature, vol 489, p 318).
That's bad news for anyone who has gone hungry for decades in the hope of living longer, but the finding has not deterred fasting researchers. They point out that although fasting obviously involves cutting calories - at least on the fast days - it brings about biochemical and physiological changes that daily dieting does not. Besides, calorie restriction may leave people susceptible to infections and biological stress, whereas fasting, done properly, should not. Some even argue that we are evolutionarily adapted to going without food intermittently. "The evidence is pretty strong that our ancestors did not eat three meals a day plus snacks," says Mattson. "Our genes are geared to being able to cope with periods of no food."
What's in a fast?
As I sit here, hungry, it certainly doesn't feel like that. But researchers do agree that fasting will leave you feeling crummy in the short term because it takes time for your body to break psychological and biological habits. Less reassuring is their lack of agreement on what fasting entails. I have opted for the "5:2" diet, which allows me 600 calories in a single meal on each of two weekly "fast" days. The normal recommended intake is about 2000 calories for a woman and 2500 for a man, and I am allowed to eat whatever I want on the five non-fast days, underlining the fact that fasting is not necessarily about losing weight. A more draconian regimen has similar restricted-calorie "fasts" every other day. Then there's total fasting, in which participants go without food for anything from one to five days - longer than about a week is considered potentially dangerous. Fasting might be a one-off, or repeated weekly or monthly.
Different regimens have different effects on the body. A fast is considered to start about 10 to 12 hours after a meal, when you have used up all the available glucose in your blood and start converting glycogen stored in liver and muscle cells into glucose to use for energy. If the fast continues, there is a gradual move towards breaking down stored body fat, and the liver produces "ketone bodies" - short molecules that are by-products of the breakdown of fatty acids. These can be used by the brain as fuel. This process is in full swing three to four days into a fast. Various hormones are also affected. For example, production of insulin-like growth factor 1 (IGF-1), drops early and reaches very low levels by day three or four. It is similar in structure to insulin, which also becomes scarcer with fasting, and high levels of both have been linked to cancer.
When it comes to treating cancer, Valter Longo, director of the Longevity Institute at the University of Southern California, thinks that short-term complete fasts maximise the benefits. He has found that a 48-hour total fast slowed the growth of five of eight types of cancer in mice, the effect tending to be more pronounced the more fasts the animals undertook (Science Translational Medicine, vol 4, p 124ra27). Fasting is harder on cancer cells than on normal cells, he says. That's because the mutations that cause cancer lead to rapid growth under the physiological conditions in which they arose, but they can be at a disadvantage when conditions changes. This could also explain why fasting combined with conventional cancer treatment provides a double whammy. Mice with gliomas - a very aggressive cancer and the most commonly diagnosed brain tumour in people - were more than twice as likely to survive the 28-day study if they underwent a 48-hour fast at the same time as radiation therapy than those without the fast (PloS One, vol 7, p e44603).
Clinical trials assessing the impact of fasting in people with cancer are ongoing. Early results are promising, says Longo, and patients in the advanced stages of cancer, who cannot wait for the results, might find it worth discussing fasting with their oncologist.
Less is more
Could fasting prevent cancers developing in the first place? Evidence is scant but there are "very good reasons" why it should, says Longo. He points out that high levels of IGF-1 and glucose in the blood, and being overweight are all risk factors for cancer, and they can all be improved by fasting. Another risk factor is insulin, says Michelle Harvie at the University of Manchester, UK. Studying women whose family history puts them at high risk of developing breast cancer, she put half of them on a diet that involved cutting calories by about 25 per cent, and half on a 5:2 fast. After six months, both groups showed a reduction in blood insulin levels, but this was greater in the fasting group. Harvie's team is now analysing breast biopsies to see whether this translates to fewer of the genetic changes associated with increased cancer risk.
High insulin is also associated with type 2 diabetes, so perhaps it is no surprise that fasting shows promise here too. At the Intermountain Heart Institute in Murray, Utah, Benjamin Horne has found that a 24-hour water-only fast, once a month, raises levels of human growth hormone, which triggers the breakdown of fat for energy use, reducing insulin levels and other metabolic markers of glucose metabolism. As a result, people lost weight and their risk of getting diabetes and coronary heart disease was reduced (American Journal of Cardiology, vol 102, p 814). Alternate day fasting (with a 500-calorie lunch for women and 600-calorie one for men on fast days) has similar benefits, says Krista Varady of the University of Illinois, Chicago. She has seen improvements in people's levels of low-density lipoprotein cholesterol, sometimes known as "bad cholesterol", and blood pressure, in volunteers eating either a low-fat or high-fat diet on "feeding" days.
For people who are overweight, any kind of intermittent fasting diet will probably help reduce the risk of diabetes and cardiovascular problems, says Mattson. In 2007, he found another benefit too. He put 10 overweight people with asthma on an alternate-day incomplete fast and found that after just a few weeks their asthma symptoms improved. Blood markers of inflammation, including C-reactive protein, also decreased, suggesting that the fast was helping to moderate their overactive immune system (Free Radical Biology and Medicine, vol 42, p 665). Whether fasting would benefit people with asthma who are in the normal weight range or those with other conditions associated with an overactive immune response, remains to be seen. There is some evidence that alternate-day fasting can lower their levels of blood fat. However, Mattson suspects that when it comes to diabetes and cardiovascular disease, fasting may not be as beneficial for people of normal weight as it is for people who are overweight, simply because they are already likely to be in pretty good shape, metabolically speaking.
Mattson has, however, identified another effect of fasting that he believes can benefit everyone - it is good for the brain. "If you look at an animal that's gone without food for an entire day, it becomes more active," he says. "Fasting is a mild stressor that motivates the animal to increase activity in the brain." From an evolutionary perspective, this makes sense because if you are deprived of food, your brain needs to begin working harder to help you find something to eat. His studies show that alternate-day fasting, with a single meal of about 600 calories on the fast day, can boost the production of a protein called brain-derived neurotrophic factor by 50 to 400 per cent, depending on the brain region. This protein is involved in the generation of new brain cells, and plays a role in learning and memory. It can also protect brain cells from the changes associated with Alzheimer's and Parkinson's (Neurobiology of Disease, vol 26, p 212). In mice engineered to develop Alzheimer's-like symptoms, alternate-day fasting begun in middle age delayed the onset of memory problems by about six months. "This is a large effect," Mattson says, perhaps equivalent to 20 years in people.
So, what about the common advice to start the day with a good breakfast? Mattson believes it is flawed, pointing out that the studies were based on schoolchildren who usually ate breakfast, meaning their poor performance could simply be due to the ill effects that occur when people begin fasting. Mattson himself skips breakfast and lunch five days a week, then has dinner and normal weekend meals with his family. Varady has tried alternate-day fasting, but she likes to eat dinner with her 18-month-old child and husband, so now keeps her food intake to within an eight hour period. Harvie, however, sounds a more cautious note for anyone thinking of giving fasting a go. "We still don't know exactly who should be fasting, how often or how many days a week," she says. Besides, it may not be without risks. One study in mice, for example, found that an alternate-day fast for six months reduced the heart's ability to pump blood (Journal of Cardiac Failure, vol 16, p 843).
There is also the fact that fasting is difficult. Varady finds that between 10 and 20 per cent of people who enrol in her studies drop out, unable to stick to the regime. This may be less of a problem in the future, though. Researchers are now investigating the possibility that you can get some of the health benefits of fasting without actually depriving yourself of food (see "Hold the protein").
As I count down the minutes to the end of my fast, I can't help wishing them success.
*********Sidebar********
Hold the protein
One key physiological effect of fasting is that it lowers levels of a hormone called insulin-like growth factor 1. Low levels of IGF-1 are associated with a decreased risk of cancer and increased lifespan. So if you could reduce it by, say, 70 per cent, wouldn't you? The only catch is that it takes five days without food to do this. But what if you could get the same result simply by altering your diet? Luigi Fontana at the University of Palermo, Italy, thinks it may be possible.
Suspecting that fasting per se is not what matters, Fontana compared the IGF-1 levels of members of the Calorie Restriction Society of Newport, North Carolina, with people who ate a typical western diet. There was no difference, despite the former group having severely reduced their calorie intake for an average of six years. However, IGF-1 levels among a group of strict vegans were significantly lower, even if they weighed more. The key, he believes, is protein, which accounted for just 10 per cent of calories for the vegans but about 25 per cent for the calorie-restricted group (Aging Cell, vol 7, p 681).
There is strong evidence linking high protein intake with cancer, says Fontana. For example, cancer rates increase for people who move from a low-protein Japanese diet to a relatively high-protein US diet. He is currently comparing the IGF-1 lowering potential of protein restriction with fasting.
Results are not yet in, but Fontana doesn't advocate eschewing protein altogether, just consuming the US recommended daily allowance of 0.8 grams per kilogram of body weight. That equates to about 10 per cent of calories from protein - in the west, protein makes up at least 16 per cent of the daily diet. The medical dogma is that lots of protein is good for you, Fontana says. "But I think it's wrong. I challenge the medical community to reconsider."
*********End Sidebar********
Emma Young is a writer based in Sheffield, UK
There was a good article on it in New Scientist a few months back. I'll post the text below. If you have access to their site it has links to some of the primary sources.
I might wait a little while until someone actually shows that it works. In the mean time -
Eat Food
Not too Much
Mostly vegetables
or even simpler
Eat less
Move more.
*************************************************************************************************************************
For a healthier body and mind, forget food fads and try the age-old practice of going without
THERE'S a fuzz in my brain and an ache in my gut. My legs are leaden and my eyesight is blurry. But I have only myself to blame. Besides, I have been assured that these symptoms will pass. Between 10 days and three weeks from now, my body will adjust to the new regime, which entails fasting for two days each week. In the meantime, I just need to keep my eyes on the prize. Forget breakfast and second breakfast, ignore the call of multiple afternoon snacks, because the pay offs of doing without could be enormous.
Fasting is most commonly associated with religious observation. It is the fourth of the Five Pillars of Islam. Buddhists consider it a means to practise self-control and advocate abstaining from food after the noon meal. For some Christians, temporary fasts are seen as a way of getting closer to God. But the benefits I am hoping for are more corporeal.
The idea that fasting might be good for your health has a long, if questionable, history. Back in 1908, "Dr" Linda Hazzard, an American with some training as a nurse, published a book called Fasting for the Cure of Disease, which claimed that minimal food was the route to recovery from a variety of illnesses including cancer. Hazzard was jailed after one of her patients died of starvation. But what if she was, at least partly, right?
A new surge of interest in fasting suggests that it might indeed help people with cancer. It could also reduce the risk of developing cancer, guard against diabetes and heart disease, help control asthma and even stave off Parkinson's disease and dementia. Many of the scientists who study fasting practise what they research, and they tell me that at my age (39) it could be vital that I start now. "We know from animal models," says Mark Mattson at the US National Institute on Aging, "that if we start an intermittent fasting diet at what would be the equivalent of middle age in people, we can delay the onset of Alzheimer's and Parkinson's." Surely it's worth a try?
Until recently, most studies linking diet with health and longevity focused on calorie restriction. They have had some impressive results, with the lifespan of various lab animals lengthened by up to 50 per cent after their daily calorie intake was cut in half. But these effects do not seem to extend to primates. A 23-year-long study of macaques found that although calorie restriction delayed the onset of age-related diseases, it had no impact on lifespan. So other factors such as genetics may be more important for human longevity too (Nature, vol 489, p 318).
That's bad news for anyone who has gone hungry for decades in the hope of living longer, but the finding has not deterred fasting researchers. They point out that although fasting obviously involves cutting calories - at least on the fast days - it brings about biochemical and physiological changes that daily dieting does not. Besides, calorie restriction may leave people susceptible to infections and biological stress, whereas fasting, done properly, should not. Some even argue that we are evolutionarily adapted to going without food intermittently. "The evidence is pretty strong that our ancestors did not eat three meals a day plus snacks," says Mattson. "Our genes are geared to being able to cope with periods of no food."
What's in a fast?
As I sit here, hungry, it certainly doesn't feel like that. But researchers do agree that fasting will leave you feeling crummy in the short term because it takes time for your body to break psychological and biological habits. Less reassuring is their lack of agreement on what fasting entails. I have opted for the "5:2" diet, which allows me 600 calories in a single meal on each of two weekly "fast" days. The normal recommended intake is about 2000 calories for a woman and 2500 for a man, and I am allowed to eat whatever I want on the five non-fast days, underlining the fact that fasting is not necessarily about losing weight. A more draconian regimen has similar restricted-calorie "fasts" every other day. Then there's total fasting, in which participants go without food for anything from one to five days - longer than about a week is considered potentially dangerous. Fasting might be a one-off, or repeated weekly or monthly.
Different regimens have different effects on the body. A fast is considered to start about 10 to 12 hours after a meal, when you have used up all the available glucose in your blood and start converting glycogen stored in liver and muscle cells into glucose to use for energy. If the fast continues, there is a gradual move towards breaking down stored body fat, and the liver produces "ketone bodies" - short molecules that are by-products of the breakdown of fatty acids. These can be used by the brain as fuel. This process is in full swing three to four days into a fast. Various hormones are also affected. For example, production of insulin-like growth factor 1 (IGF-1), drops early and reaches very low levels by day three or four. It is similar in structure to insulin, which also becomes scarcer with fasting, and high levels of both have been linked to cancer.
When it comes to treating cancer, Valter Longo, director of the Longevity Institute at the University of Southern California, thinks that short-term complete fasts maximise the benefits. He has found that a 48-hour total fast slowed the growth of five of eight types of cancer in mice, the effect tending to be more pronounced the more fasts the animals undertook (Science Translational Medicine, vol 4, p 124ra27). Fasting is harder on cancer cells than on normal cells, he says. That's because the mutations that cause cancer lead to rapid growth under the physiological conditions in which they arose, but they can be at a disadvantage when conditions changes. This could also explain why fasting combined with conventional cancer treatment provides a double whammy. Mice with gliomas - a very aggressive cancer and the most commonly diagnosed brain tumour in people - were more than twice as likely to survive the 28-day study if they underwent a 48-hour fast at the same time as radiation therapy than those without the fast (PloS One, vol 7, p e44603).
Clinical trials assessing the impact of fasting in people with cancer are ongoing. Early results are promising, says Longo, and patients in the advanced stages of cancer, who cannot wait for the results, might find it worth discussing fasting with their oncologist.
Less is more
Could fasting prevent cancers developing in the first place? Evidence is scant but there are "very good reasons" why it should, says Longo. He points out that high levels of IGF-1 and glucose in the blood, and being overweight are all risk factors for cancer, and they can all be improved by fasting. Another risk factor is insulin, says Michelle Harvie at the University of Manchester, UK. Studying women whose family history puts them at high risk of developing breast cancer, she put half of them on a diet that involved cutting calories by about 25 per cent, and half on a 5:2 fast. After six months, both groups showed a reduction in blood insulin levels, but this was greater in the fasting group. Harvie's team is now analysing breast biopsies to see whether this translates to fewer of the genetic changes associated with increased cancer risk.
High insulin is also associated with type 2 diabetes, so perhaps it is no surprise that fasting shows promise here too. At the Intermountain Heart Institute in Murray, Utah, Benjamin Horne has found that a 24-hour water-only fast, once a month, raises levels of human growth hormone, which triggers the breakdown of fat for energy use, reducing insulin levels and other metabolic markers of glucose metabolism. As a result, people lost weight and their risk of getting diabetes and coronary heart disease was reduced (American Journal of Cardiology, vol 102, p 814). Alternate day fasting (with a 500-calorie lunch for women and 600-calorie one for men on fast days) has similar benefits, says Krista Varady of the University of Illinois, Chicago. She has seen improvements in people's levels of low-density lipoprotein cholesterol, sometimes known as "bad cholesterol", and blood pressure, in volunteers eating either a low-fat or high-fat diet on "feeding" days.
For people who are overweight, any kind of intermittent fasting diet will probably help reduce the risk of diabetes and cardiovascular problems, says Mattson. In 2007, he found another benefit too. He put 10 overweight people with asthma on an alternate-day incomplete fast and found that after just a few weeks their asthma symptoms improved. Blood markers of inflammation, including C-reactive protein, also decreased, suggesting that the fast was helping to moderate their overactive immune system (Free Radical Biology and Medicine, vol 42, p 665). Whether fasting would benefit people with asthma who are in the normal weight range or those with other conditions associated with an overactive immune response, remains to be seen. There is some evidence that alternate-day fasting can lower their levels of blood fat. However, Mattson suspects that when it comes to diabetes and cardiovascular disease, fasting may not be as beneficial for people of normal weight as it is for people who are overweight, simply because they are already likely to be in pretty good shape, metabolically speaking.
Mattson has, however, identified another effect of fasting that he believes can benefit everyone - it is good for the brain. "If you look at an animal that's gone without food for an entire day, it becomes more active," he says. "Fasting is a mild stressor that motivates the animal to increase activity in the brain." From an evolutionary perspective, this makes sense because if you are deprived of food, your brain needs to begin working harder to help you find something to eat. His studies show that alternate-day fasting, with a single meal of about 600 calories on the fast day, can boost the production of a protein called brain-derived neurotrophic factor by 50 to 400 per cent, depending on the brain region. This protein is involved in the generation of new brain cells, and plays a role in learning and memory. It can also protect brain cells from the changes associated with Alzheimer's and Parkinson's (Neurobiology of Disease, vol 26, p 212). In mice engineered to develop Alzheimer's-like symptoms, alternate-day fasting begun in middle age delayed the onset of memory problems by about six months. "This is a large effect," Mattson says, perhaps equivalent to 20 years in people.
So, what about the common advice to start the day with a good breakfast? Mattson believes it is flawed, pointing out that the studies were based on schoolchildren who usually ate breakfast, meaning their poor performance could simply be due to the ill effects that occur when people begin fasting. Mattson himself skips breakfast and lunch five days a week, then has dinner and normal weekend meals with his family. Varady has tried alternate-day fasting, but she likes to eat dinner with her 18-month-old child and husband, so now keeps her food intake to within an eight hour period. Harvie, however, sounds a more cautious note for anyone thinking of giving fasting a go. "We still don't know exactly who should be fasting, how often or how many days a week," she says. Besides, it may not be without risks. One study in mice, for example, found that an alternate-day fast for six months reduced the heart's ability to pump blood (Journal of Cardiac Failure, vol 16, p 843).
There is also the fact that fasting is difficult. Varady finds that between 10 and 20 per cent of people who enrol in her studies drop out, unable to stick to the regime. This may be less of a problem in the future, though. Researchers are now investigating the possibility that you can get some of the health benefits of fasting without actually depriving yourself of food (see "Hold the protein").
As I count down the minutes to the end of my fast, I can't help wishing them success.
*********Sidebar********
Hold the protein
One key physiological effect of fasting is that it lowers levels of a hormone called insulin-like growth factor 1. Low levels of IGF-1 are associated with a decreased risk of cancer and increased lifespan. So if you could reduce it by, say, 70 per cent, wouldn't you? The only catch is that it takes five days without food to do this. But what if you could get the same result simply by altering your diet? Luigi Fontana at the University of Palermo, Italy, thinks it may be possible.
Suspecting that fasting per se is not what matters, Fontana compared the IGF-1 levels of members of the Calorie Restriction Society of Newport, North Carolina, with people who ate a typical western diet. There was no difference, despite the former group having severely reduced their calorie intake for an average of six years. However, IGF-1 levels among a group of strict vegans were significantly lower, even if they weighed more. The key, he believes, is protein, which accounted for just 10 per cent of calories for the vegans but about 25 per cent for the calorie-restricted group (Aging Cell, vol 7, p 681).
There is strong evidence linking high protein intake with cancer, says Fontana. For example, cancer rates increase for people who move from a low-protein Japanese diet to a relatively high-protein US diet. He is currently comparing the IGF-1 lowering potential of protein restriction with fasting.
Results are not yet in, but Fontana doesn't advocate eschewing protein altogether, just consuming the US recommended daily allowance of 0.8 grams per kilogram of body weight. That equates to about 10 per cent of calories from protein - in the west, protein makes up at least 16 per cent of the daily diet. The medical dogma is that lots of protein is good for you, Fontana says. "But I think it's wrong. I challenge the medical community to reconsider."
*********End Sidebar********
Emma Young is a writer based in Sheffield, UK
Dave70
Le roi est mort..
- Joined
- 29/9/08
- Messages
- 5,603
- Reaction score
- 3,279
Y'all can have your armchair theorists, book salesmen and food pyramids.
Or you can contemplate the advice from a man who actually kicked arse well into his 90's.
http://singularityhub.com/2011/02/16/jack-lalanne-made-longevity-a-simple-science/
Or you can contemplate the advice from a man who actually kicked arse well into his 90's.
http://singularityhub.com/2011/02/16/jack-lalanne-made-longevity-a-simple-science/
RobW
The Little Abbotsford Craftbrewery
- Joined
- 6/8/03
- Messages
- 1,685
- Reaction score
- 110
I've been on the 5:2 for about a month which means for 2 days a week my calorie intake is around 600, about a quarter of normal.
For the first couple of restricted days I felt hungry through the day but since then I hardly notice it.
I've lost 3-4 kilos and more importantly that fat around the middle.
I don't feel as hungry on unrestricted days and I find now I don't need to eat as much to satisfy me at mealtimes.
I don't want to lose much more and will probably go to one restricted day a week soon.
I feel better - more alert, and have more energy.
I get out of bed easier in the morning.
Also it makes it easy to have a couple of AFDs a week - something that I wouldn't usually do, and eat smaller portions which used to be difficult too.
In another month or so I will have a blood checkup and see if anything has changed there - this is what I'm really interested in.
Just out of interest how many of the naysayers out there have read the book or watched the doco?
I'd recommend it.
For the first couple of restricted days I felt hungry through the day but since then I hardly notice it.
I've lost 3-4 kilos and more importantly that fat around the middle.
I don't feel as hungry on unrestricted days and I find now I don't need to eat as much to satisfy me at mealtimes.
I don't want to lose much more and will probably go to one restricted day a week soon.
I feel better - more alert, and have more energy.
I get out of bed easier in the morning.
Also it makes it easy to have a couple of AFDs a week - something that I wouldn't usually do, and eat smaller portions which used to be difficult too.
In another month or so I will have a blood checkup and see if anything has changed there - this is what I'm really interested in.
Just out of interest how many of the naysayers out there have read the book or watched the doco?
I'd recommend it.
Airgead
Ohhh... I can write anything I like here
- Joined
- 6/4/05
- Messages
- 3,651
- Reaction score
- 1,055
Not so interested in books and docos as they always have a point to push. I mean, who is going to write a book that days "Hey look at this!..umm... well.. actually.. move along.. nothing to see here".
Some peer reviewed papers from some decently sized clinical studies would be a good start. People are working on it but as the article I posted says, the science is at very early stages. There is a plausible mechanism of action through the IGF system but no actual proof that the proposed effect is real or clinically significant
Cheers
Dave.
Some peer reviewed papers from some decently sized clinical studies would be a good start. People are working on it but as the article I posted says, the science is at very early stages. There is a plausible mechanism of action through the IGF system but no actual proof that the proposed effect is real or clinically significant
Cheers
Dave.
Similar threads
- Replies
- 3
- Views
- 5K
- Replies
- 32
- Views
- 4K